
VA Puts Abortions Ahead of Caring for Veterans
The Department of Veterans Affairs (VA) is the latest agency to flout the will of the people by focusing on politics rather than its foundational mission. Instead of ensuring America’s
Alert: Scammers are using names close to ours and using articles by CWA to appear legitimate. They are not! Make sure you use ConcernedWomen.org for any donations or contact.

The Department of Veterans Affairs (VA) is the latest agency to flout the will of the people by focusing on politics rather than its foundational mission. Instead of ensuring America’s
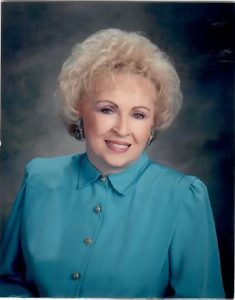
For Immediate Release April 14, 2024 Contact: CWA Communications Teamcomms@cwfa.org Tribute to CWA Founder Beverly LaHaye “A tenacious woman of God whose legacy will live on” Washington, D.C. – Concerned

For Immediate Release April 13, 2024 Contact: CWA Communications Teamcomms@cwfa.org U.S. Must Aid Israel Against Iran NOW Biden’s feckless foreign policy is putting our ally at risk Washington, D.C.

Concerned Women for America CEO and President Penny Nance is joined by Pastor of Potomac Valley Church, Will Archer, for an insightful conversation on the role of the church when

This past Sunday marked six months since the single deadliest attack against Israel with around 1,200 people brutally killed and the abduction of around 250 people – including American citizens.

“Since Mike Johnson, a man of deep faith and Christian worldview, took office in October, the House Speaker has been denounced by the Left with every radical name in the book,”
Every single cent counts, and your generosity matters. Through your donation, we are a huge step closer to empowering activist leaders and impacting entire communities and states. As we are able to deepen CWA’s impact, our nation is changed.